
Automated Medical Claims Auditing
Catch errors. Detect fraud. Optimize trust in healthcare.
BY USE CASES
The healthcare system processes millions of medical claims every day. Manual auditing is slow, expensive, and prone to human error — and traditional rule-based systems often fail to spot subtle fraud or billing anomalies.
The Challence
Healthcare claims data is:
High-volume, with thousands of daily submissions
Highly variable, due to different procedures, coding systems, and payer rules
Vulnerable to fraud, abuse, upcoding, and duplication
Difficult to audit consistently using static rules or sample-based reviews
Traditional audit systems:
Can’t scale effectively
Struggle with pattern recognition in large datasets
Rely heavily on predefined rules and thresholds, missing context
Quantum-Inspired Solution
HessQ applies quantum-inspired logic to the audit process using QUBO optimization.
Increased Accuracy
Detects more true billing anomalies and uncovers complex fraud patterns often missed by traditional audits.
Audits are completed in minutes — not hours — enabling real-time insights and faster claim decisions.
Reduces unnecessary manual reviews by minimizing false alerts, allowing teams to focus on the claims that truly matter.
Faster Processing
Fewer False Positives
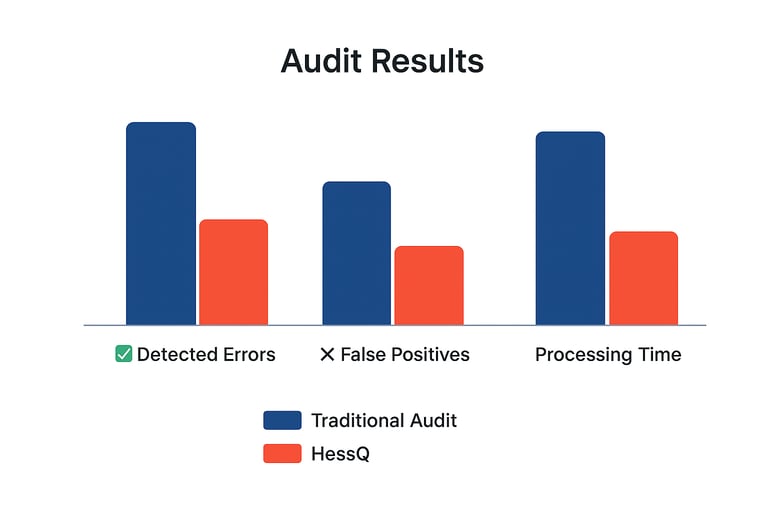
The Result:
Higher accuracy in identifying true billing anomalies
Faster processing, with results in minutes instead of hours
Fewer false positives, reducing manual review workload
Improved detection of subtle and organized fraud patterns